How Childhood Trauma Creates Adult Addicts

Addiction is extremely prevalent in the United States, affecting as many as 23.5 million Americans. These addictions are often stigmatized by society and shown as a dangerous habit of the weak-minded and the criminal. Despite this stigmatization, addiction is often significantly more complex than the media depiction, and its deep connection with trauma and abuse is well understood and documented.
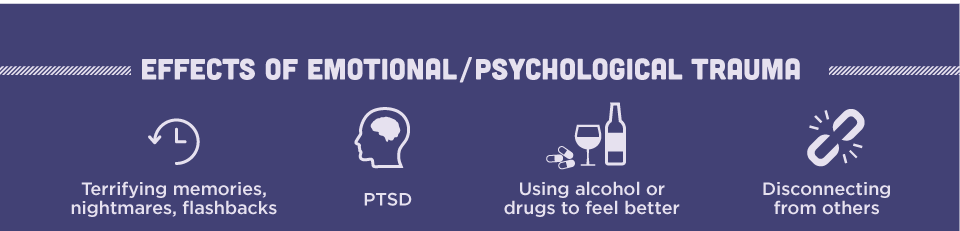
For example, more than 25% of patients who survive traumatic experiences such as car accidents, rape, or attempted murder in adulthood develop unhealthy relationships with substances. And, an average of 40% of persons with PTSD suffer from a substance use disorder.
Rates of addiction, which are already high for adult survivors of trauma, are often worse for children, whose psychological and emotional development can be severely impinged by trauma. This in turn puts children who survive trauma at a high risk of developing a substance use disorder, often as a means of coping with trauma and emotions.
The Effect of Trauma on the Brain
Developing brains are adaptable, enabling them to quickly change to meet an environment, to learn and absorb new information, and to grow at a rapid rate as they mature. In the presence of trauma, this same plasticity which enables children to absorb information from their environment to learn from it becomes harmful, because children adapt to harmful behavior, are inhibited by fear, and adapt as readily to a negative environment as they do to a positive one.
Children who have experienced trauma have been shown to have physical changes in the brain. The most well-documented include changes to the size of the Hippocampus which regulates cortisol, learning, and memory, the cingulum-hippocampus projection (CGH-R), which affects emotional regulation and processing, the corpus callosum, which is responsible for emotional regulation, the cerebellum which controls motor functions, and the prefrontal cortex which aids in behavior, cognition, and emotional regulation. Long-term stress or abuse changes the size, shape, and frequency of connections within the brain. These adaptions go on to affect the child for the rest of their adult life – even after therapy and treatment.
View Full Infographic at: Post Traumatic Stress Disorder and Addiction
As a result, children who are exposed to trauma during childhood are more likely to develop anxiety and depression and to develop an increased vulnerability to substance abuse. In one study, more than half of children who were exposed to trauma before the age of 13 were affected by either a mental disorder such as depression or by a drug or alcohol addiction or use disorder. While the study was a small one, the impact of trauma on the developing brain is undeniable.
Adverse Childhood Experiences (ACE)
There are many studies showing that trauma directly impacts negative or unhealthy behaviors such as overeating, smoking, drinking to excess, and using drugs. The ACE scale, which stands for Adverse Childhood Experiences, is shown to directly correlate with substance abuse. People with more adverse experiences are more likely to have mental and physical health problems and to use drugs and alcohol to self-medicate. In one study including over 17,000 people, adverse childhood experiences such as abuse (emotional, physical, and sexual), addicted parents, mentally ill parents, parental incarceration, neglect, domestic violence (towards family members or self), and losing a parent to death or divorce all increased the chances of the child growing up to be an addict.
This study was used to develop the ACE score, which highlights a person’s risk of developing addictive behaviors based on their background and history.
Using Substances as a Coping Mechanism

Children who are exposed to trauma often have their normal growth interrupted and are forced to adapt to a new reality. Because young children cannot create a frame of reference in which to contextualize experiences such as loss, abuse, or even a car accident, they can begin to self-medicate, to act out, and to use outside factors to soothe fears and to make themselves feel better. For example, food, safety blankets, clinging to a parent, etc., can all be used to soothe fears. These ‘innocent’ self-medications can become alcohol, drugs, or pain pills as the child grows older, more rebellious, and more aware that they are in pain.
In short, substance use is often an unhealthy response to natural needs for comfort, relief, or even feeling ‘normal’. Many survivors of trauma struggle with handling stress and negative emotions, simply because they were never given the opportunity to develop healthy coping mechanisms.
This also affects self-esteem and personal growth and development. Children who were subjected to abuse or trauma also typically suffer from lower self-esteem, which can push them to seek out substances for ‘support’ or ‘normalization’ in social and high-stress situations. For example, children who have survived trauma are more likely to use drugs or alcohol as a social crutch, rather than as a means of enjoying themselves.
Dual Diagnosis in Addicts
Adults who suffer from trauma who are driven into addiction are typically treated for post-traumatic stress disorder (PTSD because it is often the underlying cause of the addiction. Children who suffer from traumatic experiences who go on to become adult addicts are somewhat more complex, because they may be suffering from PTSD or from changes in brain development and learning which affect their ability to live normally. In order to be properly treated, adult addicts with traumatic experiences must be able to discuss their problems with a therapist who can correctly diagnose their specific problems to create a custom treatment plan that works for the individual.
Because of the high prevalence of childhood trauma and other forms of PTSD in addicts, many treatment professionals use trauma screening and therapy to recognize when adult patients have more than one diagnosis. A patient with both an addiction and PTSD from childhood trauma is described as comorbid, or having a dual diagnosis.
Dual diagnosis is important, because without it, recovery is rarely successful. Patients who go through rehab with an unrecognized dual diagnosis will likely quickly return to using after they leave and will have to go through treatment again because they haven’t developed coping skills to manage life without the substance.
This necessitates a smarter approach to therapy, in which the PTSD and effects of the trauma are treated first, before the addiction. Therapies like Cognitive Behavioral Therapy (CBT) and Dialectical Behavioral Therapy (DBT) typically create a focus in which life threatening behaviors such as physical addiction are handled first, after which the problems preventing the person from recovering from their addiction, such as PTSD, are treated. When those factors are at a manageable level, the addict receives treatment for their addiction, so that they can learn healthy coping mechanisms and life skills that will allow them to live substance free.
Getting Help
While not everyone with a substance abuse problem suffered from trauma as a child, as many as 2/3rds of addicts in some screenings have. The National Child Traumatic Stress Network also reports that as many as 60% of all children are exposed to childhood trauma, which can go on to impact their development and coping mechanisms. Many people are exposed to harmful and negative experiences during their childhood, which does impact growth and development.
Getting help means seeking out a rehabilitation center that can treat the trauma and pain at the root of an addiction, rather than just treating the addiction. This means looking for a center that offers therapy, personal care, skills development, coping mechanism development, and stress management. These skills, while not directly related to getting clean or sober, will allow an addicted person to build up a foundation with which they can use to stay clean because they no longer need drugs or alcohol to function.
If you or a loved one are suffering from an addiction, it is crucial to get help. Seeking out a rehabilitation clinic that can provide the therapy necessary to identify trauma and treat it will help. A quick action might save your life or the life of your loved one. Please contact-us Beginnings Treatment Centers now to speak with a professional who cares. We can help.


